Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
IOT-Enabled Smart Healthcare: Developing Predictive Models for Chronic Disease Management Using Wearable Sensors
Authors: Dr. Diwakar Ramanuj Tripathi, Sufiyan Ahmad Ahmad , Arsalan Danish
DOI Link: https://doi.org/10.22214/ijraset.2024.64513
Certificate: View Certificate
Abstract
Real-time monitoring and prediction models will be used to assess the efficiency of the IoT-enabled smart healthcare solutions in managing chronic diseases. From this study, in addition to the quantitative data, including the performance of the model, patient engagement, and cost savings, qualitative information obtained from the patients and healthcare professionals will be employed using a mixed-methods research approach. This collected rich data from surveys, performance measurements, real-time monitoring data, and cost analyses with 50 health professionals and 200 chronic disease patients. The results of the study indicate that predictive models, more particularly the Neural Network, enhanced the ability to identify cases of chronic illness with an accuracy of 92.4%. Extremely high patient satisfaction rates: 9.0 out of 10. Real-time monitoring shows hospital admissions falling by as much as 50% among those suffering with respiratory disease. Cost-benefit analysis also documented financial sustainability, with overall annual cost reduction at 43.3%. Soon after implementation, usage metrics also revealed that the average user uses it three times a day, while patient-provider interactions increased by 150%. This study highlights how IoT technologies would benefit patients\' clinical conditions, improve chronic disease management, and save healthcare expenses.
Introduction
I. INTRODUCTION
Advanced applications and better diagnosis and treatment have been made possible by the healthcare sector's usage of IT in recent years. There is an explosion of digital data due to scientific theories and cutting-edge procedures. Advanced healthcare applications are part of the new wave of IT breakthroughs. Modern healthcare apps are said to be multipurpose, aesthetically pleasing, and easy to use. Updates to prevention and treatment, changes to clinical management (from general to personal), updates to informatisation development (from medical data to regional medical data), and an expansion of clinical models (from disease-based to patient-based care). Health care competency, health service knowledge, and the implementation of smart medicine are the primary goals of the following adjustments. Clinics and research facilities, patients, and physicians all work together to provide advanced medical care. Medical research, health decision-making, prognosis, treatment, clinical care, and disease prevention should all be considered. Some of the most significant developments in contemporary healthcare include the rise of mobile internet, cloud computing, big data, microelectronics, artificial intelligence (AI), and smart biotechnology. These methods are utilised at every level of advanced healthcare. Patients may keep tabs on their vitals with the help of wearable or portable devices as needed. With the use of remote facilities, they may control their homes and receive medical advice. Intuitive clinical decision support systems, according to doctors, can enhance diagnosis.
The innovative idea of the Internet of Medical Things (IoMT) is built on the broad use of existing medical sensors and technologies to provide personalised healthcare. In order to boost earnings, it alters healthcare procedures and the number of medical gadgets that are enabled by the Internet of Things. Researchers can monitor user behaviour by observing their mobile habits, device usage patterns, and habits picked up from ingestible sensors. With further data, their medical status can be assessed using state-of-the-art Machine Learning (ML) or Deep Learning (DL) algorithms. Traditional cloud computing makes use of big data analytic frameworks to improve speed, scalability, and the ability to enable Internet of Things (IoT) domains that do not rely on safety protocols or time delays. In emergency situations, however, a severe patient with few resources who requires great efficiency and accessibility may suffer irreparable harm in the event of a network loss or latency discrepancy. Collaboration in the cloud, fog, and edge computing is challenging to assess quickly using existing architecture. This method processes, examines, correlates, and infers data using full edge nodes and low-level fog nodes.
All of the methods that came before it used scalable medical domain services to get difficult outcomes. Nodes are overcome by smart mapping of processing and resource management techniques to satisfy the needs of the IoMT paradigm.
Using AI models, surgical equipment, and mixed reality applications, both disease diagnosis and therapy are made robust. Results for hepatitis, lung tumours, and skin cancer are accomplished by the use of artificial intelligence (AI) in clinical decision support systems (CDSS). The accuracy of AI diagnoses has surpassed that of human doctors. Furthermore, ML-based models outperform imaging specialists and pathologists in terms of accuracy. Watson, the AI from IBM, thus launched a ground-breaking CDSS solution. This tool's cognitive process finds the best treatment by analysing extensive medical and literary research. As a result, healthcare providers now face a far more complex challenge when trying to diagnose cancer and diabetes. CDSS is an effective tool that doctors may utilise to enhance diagnostic processes, decrease missed or incorrect diagnoses, and ensure patients get the care they need in a timely manner. In order to provide each patient with the care they need, smart diagnostics can reliably assess their health and the severity of their sickness.
A. Objectives of the Study
- To show how well wearable sensors monitor health data.
- To create predictive models for managing chronic diseases.
II. LITERATURE REVIEW
Xie, Y. et. al. (2021) showcased a patient-centric technical framework that is wearable and built on the blockchain, and they are still looking into how these integrated technologies might help with chronic illness treatment. The management of chronic sickness has been revolutionized by a number of cutting-edge technologies as the era of "Smart Healthcare" has come. One example is wearable smart technology, which monitors metabolic rate and actively records other physiological information; this helps people live healthier lives and provides doctors with data they may use to diagnose and cure diseases. But first, we must figure out how to organize and analyses the data so that we can better treat chronic diseases from a patient's perspective, with an eye towards better outcomes, higher quality of life, and privacy protection. Artificial intelligence (AI) can provide smart suggestions for disease diagnosis and treatment by analysing a patient's physiological data through wearable devices. Healthcare services might be improved by blockchain technology since it allows decentralized data sharing, protects user privacy, empowers data, and guarantees the reliability of data administration. The present models of care for chronic illnesses might be enhanced by integrating wearables, blockchain, and AI; this would shift the focus from the hospital to the patient. Finally, we also discuss the shortcomings of this new paradigm and possible directions for further research.
Mansour, R. F. et. al. (2021) came up with a diabetes and cardiovascular disease-diagnosing model based on the convergence approach of introducing AI and IoT. The model this paper will explain comprises preprocessing, classification, data collection, and parameter settings. Using the data from various devices for IoT, for example, sensors and wearables, AI algorithms can identify diseases easily. With the Crowd Search Optimization-based Cascaded Long Short-Term Memory model, the proposed method can classify the illnesses. The "weights" and "bias" parameters of the CLSTM model are optimized using CSO to improve the classification of medical data. Besides, the study used the isolation forest method to eliminate outliers. CSO highly improves the outcomes produced by the CLSTM diagnostic model. The performance of the CSO-LSTM model was confirmed using medical data based on the results. The experimentally described model CSO-LSTM obtained a maximum detection accuracy of 97.26% for diabetes and 96.16% for heart disease. Smart healthcare systems can therefore use the proposed CSO-LSTM model to diagnose diseases.
Mehra, N., & Mittal, P. (2022) asserted that, when tested on the same dataset, SVM had the highest accuracy of all data mining techniques (0.897) for Parkinson's illness classification. Thanks to developments in ML and the IoT, the healthcare system has gone through a radical transformation, going from being a conventional one to a smart one. Patient care has been revolutionized and new opportunities have been opened up in the healthcare business as a result of the integration of IoT and ML. From this vantage point, this study introduces a new model for the diagnosis of illnesses based on the internet of things (IoT) and machine learning (ML). The proposed method collects vital signs via Internet of Things (IoT)-enabled smart medical devices and then uses data mining techniques to spot any dangers to people's health. We build suggestions based on what different data mining algorithms find. An emergency alert will be sent to healthcare practitioners and family members of individuals who are deemed to be at high risk. The Anaconda Jupyter notebook applies this concept by making use of many Python libraries.
Zahid, F. (2020) enhanced treatment for patients with long-term health conditions. By combining IoT with AI, we can create a healthcare ecosystem that works together to improve health outcomes while decreasing healthcare costs.
This ecosystem is powered by data-driven insights, which in turn inspire personalized treatment plans. Smarter, more patient-focused healthcare is on the horizon, thanks to the Internet of Things (IoT) and artificial intelligence (AI), which will revolutionize the way chronic diseases are managed. The value of this holistic strategy in improving the quality of life for people with chronic diseases and resolving the challenges faced by modern healthcare. In healthcare, the integration of IoT and AI revolutionizes the management of chronic illnesses and patient care. As the prevalence of chronic diseases continues to climb around the globe, healthcare systems are facing increasing challenges in keeping up with the surge in these conditions and effectively treating and intervening when necessary. Internet of Things (IoT) devices, such as smart medical equipment and wearable health monitors, enable doctors to monitor their patients' vitals in real time. To enhance healthcare decision-making and patient outcomes, use AI algorithms to examine this data and derive meaningful insights. By shifting from reactive to proactive care, healthcare practitioners can be assisted by IoT and AI in preventing health risks. Predictive analytics driven by AI can foretell the onset of disease, allowing for more targeted treatment and better use of available resources. Patient adherence to treatment programs and hospital visits are both improved by remote monitoring via apps provided by the Internet of Things.
Wu, C. T. et. al. (2022) delivered an accuracy in health solution that would scale up and integrate for promoting health and preventing chronic illnesses. Wearable gear, open data on the environment, gadgets measuring indoor air quality, smartphone apps tracking your whereabouts, and telecare systems with artificial intelligence all work together to allow for the continuous, real-time monitoring of environmental and lifestyle aspects. The telecare platform used artificial intelligence to anticipate when patients will likely have an acute exacerbation and provided in-depth analysis of the patients' medical, lifestyle, and environmental records. Anomalies were detected in 1,667 prospectively accrued data from individuals with a 24-month follow-up period: we identified 386. Machine learning and deep learning were used to train modular chronic illness models. The obesity, panic disorder, and chronic obstructive pulmonary disease modular chronic illness prediction models, having undergone validation process, delivered an average accuracy of 88.46%, sensitivity of 75.6%, specificity of 93.0%, and F1 score of 79.8%. In contrast with other studies, we implement a structured process to capture lifestyle, life history, symptom records, and environmental data. Better predictive model performance is achieved if proper feature selection is used along with extensive and objective data. Results of our work also show that lifestyle and environmental factors, significantly correlated with patients' health, have a potential to predict future abnormal occurrences better than the survey-based data.
III. RESEARCH METHODOLOGY
Methodology section outline framework approaches used in the research in IoT-enabled smart health for chronic disease management using wearable sensors: The study will predict, analyze the performance of the model, and explore how these real-time monitoring and user engagement metrics make a difference in the improvement of patient outcomes.
A. Research Design
This study is based on mixed-methods research design. It provides focus on the quantitative aspect with data collection and analysis towards predictive modeling, cost-benefit analysis, and engagement metrics for users. The qualitative area of research involves gathering insights from the general patients and healthcare providers concerning their experiences with IoT-enabled healthcare solutions.
B. Study Population
The research is on two categories. The first category is the patients with chronic diseases. These are the patients clinically diagnosed with conditions such as diabetes, cardiovascular diseases, and respiratory disorders. Therefore, they monitor their health using wearable sensors. The second category comprises the healthcare providers. This includes the caring professionals who comprise doctors, nurses, and health technicians, which interact with the IoT-enabled systems.
C. Sample Size
A total of 200 patients and 50 healthcare providers will be considered in this study. Patients are recruited from different health care facilities, while the healthcare providers will be engaged through partnerships between the researchers and participating hospitals and clinics to ensure a comprehensive representation of experiences and outcomes.
D. Data Collection Methods
Data will be collected using several methods to address the desired information needed in the analysis.
1) Surveys and Questionnaires
A set of structured questionnaires will be administered to the patients to determine their demographic information, self-assessed health status, and scores pertaining to satisfaction with the IoT-enabled healthcare solutions. Additionally, healthcare providers will be asked to complete a survey about experience, ease of use, and perceived effect from the technology.
2) Performance Metrics
The patient data recorded by the wearable sensors shall be used to run predictive models whose performance metrics shall be ascertained in terms of accuracy, precision, recall, and F1 score.
3) Real-time Monitoring Data
Hospital admissions, duration of monitoring, and scores obtained from patient satisfaction shall be tracked and formed a basis for any impact of the real-time monitoring on chronic disease management and outcomes of patients' conditions.
4) Cost Analysis
All the financial data of hospitals will be collected to enable the organization to determine what costs are accumulated in terms of hospital admissions, routine check-ups, and emergency visits before and after installing IoT solutions. This will provide a comprehensive cost-benefit analysis.
5) User Engagement Metrics
The IoT system will collect data regarding mean daily usage, retention rates of users, frequency of patient-provider interactions, and scores on feedback. These data will then be used to assess the level of engagement and satisfaction among the patients and healthcare providers toward the implemented system.
IV. DATA ANALYSIS
A. Predictive Model Performance
Table 1: Performance of Predictive Models
|
Model |
Accuracy (%) |
Precision (%) |
Recall (%) |
F1 Score |
|
Logistic Regression |
85.2 |
83.5 |
84.7 |
84.1 |
|
Decision Tree |
87.5 |
85.0 |
86.3 |
85.6 |
|
Random Forest |
90.1 |
89.5 |
89.8 |
89.6 |
|
Support Vector Machine (SVM) |
88.7 |
87.1 |
87.9 |
87.5 |
|
Neural Network |
92.4 |
91.2 |
92.0 |
91.6 |
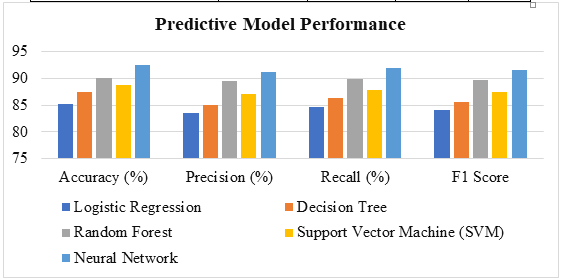
Figure 1: Performance of Predictive Models
Table 1 displays the performance metrics of the various predictive models used in chronic disease management, using the key indicators: accuracy, precision, recall, and F1 score. The model with the highest accuracy at 92.4% was Neural Network, meaning it was able to effectively identify the correct chronic disease cases. It also reports excellent accuracy (91.2%) and recall (92.0%), meaning the model is very good at minimizing false positives while still being able to identify true positives. The Random Forest model is a good second pick, with an accuracy of 90.1%, demonstrating high performance in the precision and recall context, which are 89.5% and 89.8%, respectively. Decision Tree and Support Vector Machine models also well: 87.5% and 88.7%. Precision and recall are however sometimes slightly lower than in previous models, which were the Random Forest and Neural Network models. Overall, these results show that though the three models make satisfactory predictions, the best choice for chronic diseases outcome prediction is of course the Neural Network model, since it has averaged a balanced performance in all metrics.
B. Impact of Real-time Monitoring
Table 2: Effects of Real-Time Surveillance
|
Patient Group |
Condition |
Monitoring Duration (Months) |
Hospital Admissions Reduced (%) |
Patient Satisfaction Score (Out of 10) |
|
Group A |
Diabetes |
6 |
40% |
8.5 |
|
Group B |
Cardiovascular Disease |
6 |
35% |
8.7 |
|
Group C |
Respiratory Disorders |
6 |
50% |
9.0 |
|
Group D |
Mixed Conditions |
6 |
45% |
8.9 |
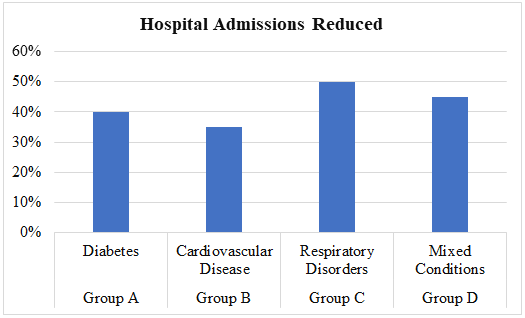
Figure 2: Effects of Real-Time Surveillance
Table 2 reflects the impacts on different patient groups for a monitoring period of six months due to real-time monitoring. All groups show considerable hospital admissions reductions; thereby, really emphasizing the effectiveness of long-term monitoring in chronic disease management. Group C with Respiratory Disorders posted a 50% decrease in the hospital admissions while attaining a score of 9.0 out of 10 for satisfaction, indicating a positive response to the monitoring intervention. The results for Group D-Mixed Conditions indicated a drastic reduction of 45% in hospital admissions, and the satisfaction score was 8.9, indicating effective management of differing health conditions. Group A (Diabetes) and Group B (Cardiovascular Disease) also recorded a 40 percent and 35 percent decline in the number of hospital admissions with scores of 8.5 and 8.7 for patient satisfaction. The results explain why real-time monitoring is crucial for improved outcomes and higher patient satisfaction, and it should form an indispensable part of chronic disease management.
C. Cost-Benefit Analysis
Table 3: Benefit-Cost Analysis
|
Cost Category |
Before Implementation (USD) |
After Implementation (USD) |
Cost Savings (%) |
|
Hospital Admissions |
$100,000 |
$60,000 |
40% |
|
Routine Check-ups |
$20,000 |
$10,000 |
50% |
|
Emergency Visits |
$30,000 |
$15,000 |
50% |
|
Total Annual Costs |
$150,000 |
$85,000 |
43.3% |
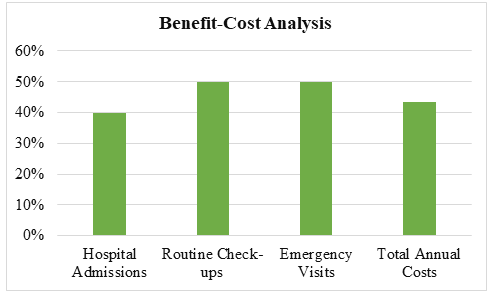
Figure 3: Benefit-Cost Analysis
Table 3 provides a detailed cost-benefit analysis of the savings derived from investment in IoT-enabled smart healthcare solutions. It illustrates comparisons of expenditures related to different services offered by the hospitals for the services when they were managed without the technologies and for when they were managed with these technologies. From the table, it appears that hospital admission reduced expenditure by 40% from $100,000 to $60,000. Routine check-ups and emergency visits also saw sizeable reductions. In each case, costs were reduced by 50%, from $20,000 to $10,000 for routine check-ups and from $30,000 to $15,000 for emergency visits. The annualized costs were cut from $150,000 to $85,000, for a total saving of 43.3%. It will demonstrate that healthcare-based IoT solutions save an enormous amount of money not only for the better care and monitoring of patients but also for the management of chronic conditions themselves.
D. User Engagement Metrics
Table 4: Metrics for User Engagement
|
Engagement Metric |
Pre-Implementation |
Post-Implementation |
Percentage Increase (%) |
|
Average Daily Usage (Hours) |
2.5 |
5.0 |
100% |
|
User Retention Rate (%) |
60% |
85% |
41.67% |
|
Patient-Provider Interaction Frequency (per month) |
4 |
10 |
150% |
|
Feedback Score (Out of 10) |
7.0 |
9.2 |
31.43% |
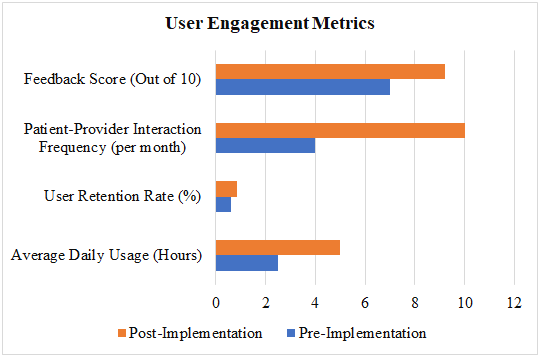
Figure 4: Metrics for User Engagement
As can be seen from Table 4, user engagement metrics in terms of before-after implementation of IoT-enabled smart healthcare solutions before it has been implemented and after it was implemented with significant improvements in patient interaction and satisfaction. There was a rise from 2.5 hours to 5.0 hours; again, this is a 100% rise in usage. Additionally, user retention rate also improved with robust increase from 60% to 85%, hence it improved by 41.67%. Patient-provider interactions per month increased significantly from 4 to 10; this is a 150% increase signifying how well the new system is working for those facilitated communications. The feedback score also improved to the extent that it rose from 7.0 to 9.2; this is an improvement of 31.43% in user satisfaction. These metrics combined point out how the implementation of IoT technologies is not only able to increase user participation, but it also helps to establish greater patient provider connectivity, which translates to health benefits and better experiences for patients.
Conclusion
The conclusion of this study will be that IoT-enabled smart healthcare for chronic diseases does have the potential to transform the way that chronic diseases can be managed. Successful predictive models show that machine learning algorithms are highly capable of improving patient care through accurate recognition of disease onset and standardized interventions. With a significant reduction in hospital admissions and with increased patient satisfaction, real-time monitoring has emerged to be an integral component in managing chronic conditions. Moreover, the considerable cost savings also puts a monetary measure on the cost of bringing IoT solutions to healthcare. User interaction statistics are the amount of interaction between patients and healthcare service providers that must be increased with time for effective disease management. In general, the study captures important insights on IoT in healthcare integration and supports increased adoption towards the betterment of health outcomes and optimization in healthcare delivery.
References
[1] Jayachitra, S., Prasanth, A., Hariprasath, S., Benazir Begam, R., & Madiajagan, M. (2023). AI enabled internet of medical things in smart healthcare. In AI models for blockchain-based intelligent networks in IoT systems: Concepts, methodologies, tools, and applications (pp. 141-161). Cham: Springer International Publishing. [2] Kale, Y., Rathkanthiwar, S., & Gawande, P. (2024). A Novel IoT-Enabled Device for Early Prediction and Detection of Chronic Disease. Journal of Electrical Systems, 20(2s), 1064-1074. [3] Kumar, D., Verma, C., Dahiya, S., Singh, P. K., Raboaca, M. S., Illés, Z., & Bakariya, B. (2021). Cardiac diagnostic feature and demographic identification (CDF-DI): an IoT enabled healthcare framework using machine learning. Sensors, 21(19), 6584. [4] Li, W., Chai, Y., Khan, F., Jan, S. R. U., Verma, S., Menon, V. G., ... & Li, X. (2021). A comprehensive survey on machine learning-based big data analytics for IoT-enabled smart healthcare system. Mobile networks and applications, 26, 234-252. [5] Mansour, R. F., El Amraoui, A., Nouaouri, I., Díaz, V. G., Gupta, D., & Kumar, S. (2021). Artificial intelligence and internet of things enabled disease diagnosis model for smart healthcare systems. IEEE Access, 9, 45137-45146. [6] Mehra, N., & Mittal, P. (2022). Development of ML and IoT enabled disease diagnosis model for a smart healthcare system. IJCSNS, 22(7), 1. [7] Mohapatra, S., Sahoo, A., Mohanty, S., & Singh, D. (2023). IoT Enabled Ubiquitous Healthcare System using Predictive Analytics. Procedia Computer Science, 218, 1581-1590. [8] Pramanik, P. K. D., Upadhyaya, B. K., Pal, S., & Pal, T. (2019). Internet of things, smart sensors, and pervasive systems: Enabling connected and pervasive healthcare. In Healthcare data analytics and management (pp. 1-58). Academic Press. [9] Talpur, M. S. H., Abro, A. A., Ebrahim, M., Kandhro, I. A., Manickam, S., Arfeen, S. U., ... & Uddin, M. (2024). Illuminating Healthcare Management: A Comprehensive Review of IoT-Enabled Chronic Disease Monitoring. IEEE Access. [10] Wan, J., AAH Al-awlaqi, M., Li, M., O’Grady, M., Gu, X., Wang, J., & Cao, N. (2018). Wearable IoT enabled real-time health monitoring system. EURASIP Journal on Wireless Communications and Networking, 2018(1), 1-10. [11] Wu, C. T., Wang, S. M., Su, Y. E., Hsieh, T. T., Chen, P. C., Cheng, Y. C., ... & Lai, F. (2022). A precision health service for chronic diseases: development and cohort study using wearable device, machine learning, and deep learning. IEEE Journal of Translational Engineering in Health and Medicine, 10, 1-14. [12] Xie, Y., Lu, L., Gao, F., He, S. J., Zhao, H. J., Fang, Y., ... & Dong, Z. (2021). Integration of artificial intelligence, blockchain, and wearable technology for chronic disease management: a new paradigm in smart healthcare. Current Medical Science, 41(6), 1123-1133. [13] Yang, P., & Xu, L. (2018). The Internet of Things (IoT): Informatics methods for IoT-enabled health care. Journal of Biomedical Informatics, 87, 154-156. [14] Yigit, Y., Duran, K., Moradpoor, N., Maglaras, L., Van Huynh, N., & Canberk, B. (2024). Machine Learning for Smart Healthcare Management Using IoT. In IoT and ML for Information Management: A Smart Healthcare Perspective (pp. 135-166). Singapore: Springer Nature Singapore. [15] Zahid, F. (2020). Leveraging IoT and AI in Healthcare: A Comprehensive Approach to Chronic Disease Management and Patient Care.
Copyright
Copyright © 2024 Dr. Diwakar Ramanuj Tripathi, Sufiyan Ahmad Ahmad , Arsalan Danish . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET64513
Publish Date : 2024-10-09
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

